Theory of Change
In rural Ghana, persistent disparities in access to maternal healthcare are primarily due to a weak healthcare system. This is exacerbated by delays in seeking and receiving obstetric care due to limited knowledge and decision-making capacity amongst women and adolescent girls. Additionally, gender disparities, cultural barriers, and illiteracy hinder positive maternal and infant health (MIH) outcomes. We will scale up and evaluate four successful educational and empowerment interventions that leverage data and technology. Our target audience includes healthcare workers, adolescent girls, pregnant women, postpartum women, women’s partners and husbands in 25 rural communities.
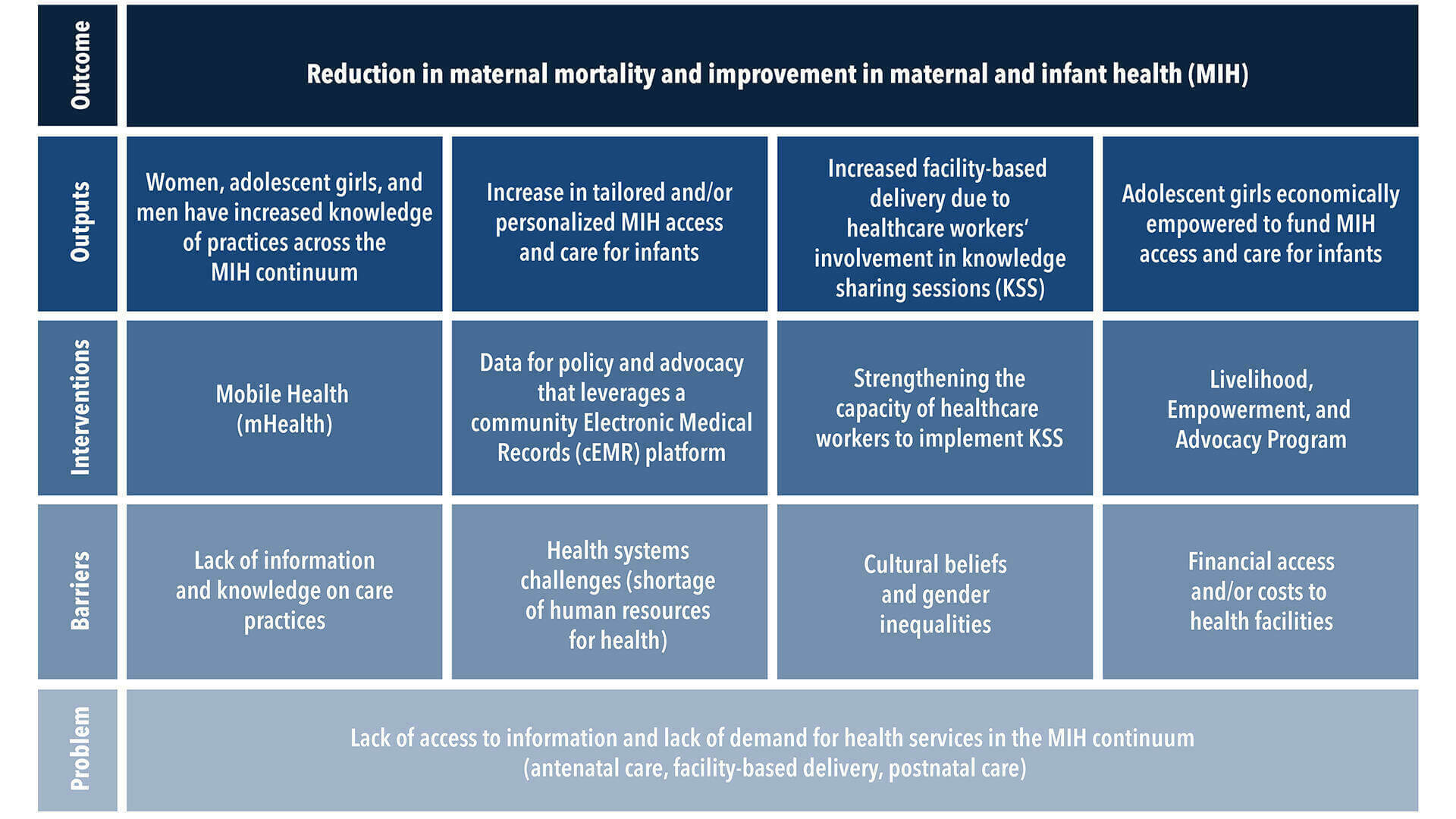 Theory of change, click to zoom in.
Theory of change, click to zoom in.- The mHealth intervention allows bidirectional exchange of MIH information and questions in English and local languages through voice or text formats. Information shared via mHealth also reinforces KSS messages and highlights details that can improve MIH in local communities.
- The cEMR platform used by healthcare workers to inform interventions and personalize health information for women and adolescent girls will employ data analytic strategies to ensure data-driven decision making, especially for those who are at the highest risk for poor health outcomes.
- Strengthening facility-based and community healthcare workers’ information and communications technology (ICT) capacity through tailored and iterative training, including mHealth and cEMR, will facilitate the design and delivery of health education to women and their families.
- The LEAP for adolescent girls facilitates entrepreneurship, provides educational sessions for income generation, as well as health education so that participants have increased access to MIH services.
Outcomes of the T4MIH package of interventions include increased MIH knowledge, timely health-related decision-making, and greater access to skilled MIH services. Additionally, adolescent girls are more empowered with higher capacity to provide for themselves and their infants. Partners and husbands also have increased knowledge and higher capacity to support women and infants, while healthcare workers are more equipped to lead KSS and to tailor health messages for women, adolescent girls, and partners. The sustained impacts that our project will have are 1) improved MIH outcomes, 2) greater professional capacity among healthcare workers to apply data analytics and information in influencing health behavior and practices, 3) more knowledgeable and supportive partners/husbands who can identify harmful cultural practices, gender disparities and understand women’s needs, and 4) financial independence among adolescent girls.